UMSON Researcher Partners with UMMC Nurse Practitioner and UMSON Alumna
January 05, 2024 Giordana Segneri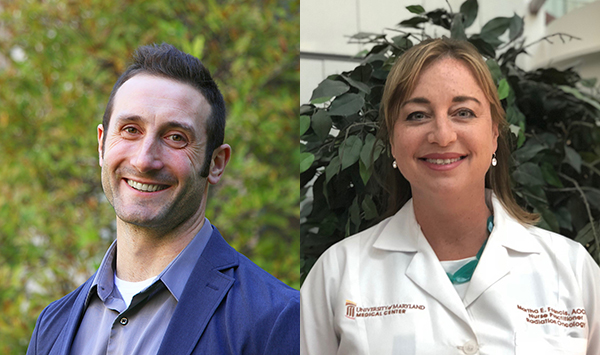
Associate professor awarded collaborative UMNursing grant for research into effectiveness of Serious Illness Conversation Guide with intimate partners facing lung cancer.
The University of Maryland School of Nursing’s (UMSON) Ian Kleckner, PhD, MPH, associate professor and director of UMSON's SYNAPSE Center, has received a one-year, $15,000 UMNursing grant, a joint venture between UMSON and the University of Maryland Medical Center (UMMC), for the project “Phase 1 Feasibility Testing of Serious Illness Conversation Guide in Patients and Intimate Partner Dyads Living with Advanced Cancer.” Kleckner (pictured, left) has partnered with Martha E. Francis, PhD '21, RN, FNP-BC, CRNP, AOCNP, (right) nurse practitioner at UMMC, to conduct the research.
In addition, the UMNursing grant provides $2,500 for each of the researchers, to be allocated based on requests over the course of the 12-month period.
Being diagnosed with advanced lung cancer has a profound impact on patients and their families, leaving them feeling unstable and vulnerable, further influencing their ability to communicate openly together during the illness experience. Hope is a commonly used coping behavior to lessen distress and remain positive when contemplating the future with lung cancer.
Preliminary research on intimate partner dyads (patient and intimate partner couples) living with advanced cancer revealed that embracing hope and positivity was an unseen barrier for dyads to share emotionally vulnerable content (fears, values, goals, and care preferences) together during the illness.
The Serious Illness Conversation Guide (SICG) has been tested and shown to be effective in supporting serious illness conversations between providers and patients and resulted in improved outcomes in end of life. It is not yet known if the SICG can be used with intimate partner dyads and delivered early after diagnosis. Although patients have demonstrated improved outcomes following the SICG intervention, it is unclear if including intimate partners will improve psychosocial outcomes for both members of the dyad during the illness.
The long-term goal of this proposed research is to optimize interventions to support open communication of emotionally vulnerable content for intimate partner dyads living with advanced cancer, resulting in moderate to large effects on psychosocial outcomes for the dyad through illness, death, and bereavement.
The first step in this goal was a multi-method study by Francis to investigate intimate partner communication with a specific focus on how couples shared their illness experience and other emotionally vulnerable content with each other while living with an advanced cancer. This same study also explored relationships between dyadic communication and suffering during illness.
Results revealed that dyads explicitly requested assistance with these difficult conversations and that difficulty communicating together increased suffering during cancer. The second step is to test a validated communication tool (SICG) early after diagnosis and with intimate partner dyads, which will lead to future federal funding awards to investigate this problem more definitely.
- Aim 1 will test the feasibility and acceptability of the SICG tool with intimate partner dyads early after a diagnosis of advanced lung cancer.
- Aim 2 will assess the effects of the SICG tool on depression, quality of life, and suffering at baseline, six, and 12 weeks following the intervention.
This study is the first to use SICG in intimate partner dyads, early after diagnosis, and is novel in its foundation of dyadic theory. Before dyads can share values and preferences with health care providers, they must first have had the opportunity to navigate these vulnerable conversations with each other. Supporting open communication of vulnerable aspects of one’s illness experience may be ‘low tech,' but it transcends all that separates us and has profound potential to impact outcomes, extending improvements well beyond the dyad to external family, providers, and institutions.