Rooted in History: 1891 UMSOM Alum at Center of Pivotal Yellow Fever Research
August 19, 2024 Tara Wink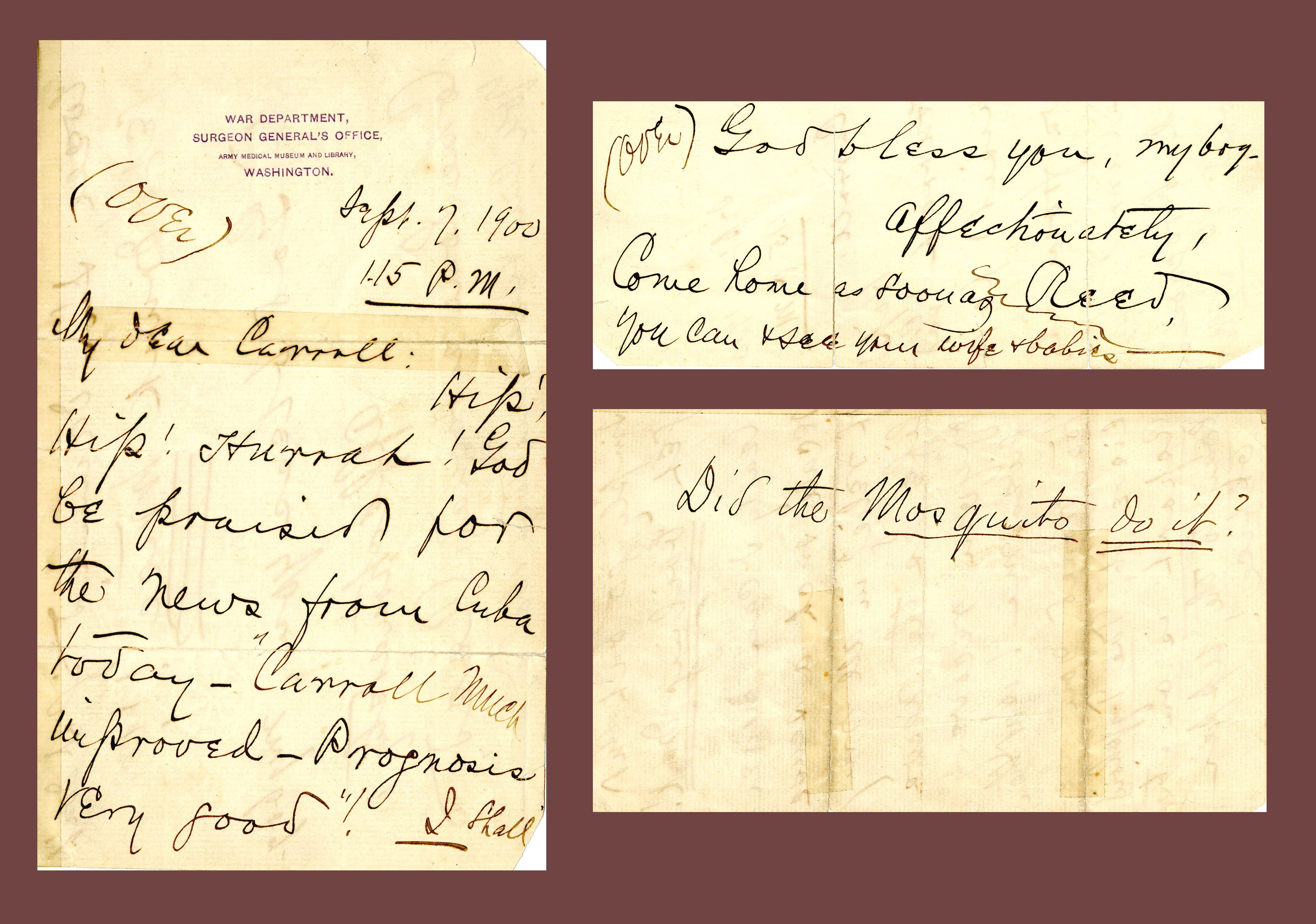
Dr. James Carroll, who was infected through a mosquito bite in 1900 and recovered, served on the Yellow Fever Commission in Cuba.
Photo: On Sept. 7, 1900, after hearing that Dr. James Carroll, an 1891 UMSOM graduate, was improving from yellow fever, Walter Reed wrote him asking, “Did the Mosquito do it?”
Over hundreds of years, ships entering the Baltimore harbor have carried with them not only people and goods but also diseases.
Yellow fever was a particularly common epidemic in the 18th and 19th centuries in the port city of Baltimore. Because the University of Maryland School of Medicine (UMSOM) is in the heart of the city, its students and faculty saw the firsthand effects of the disease, resulting in a long history of yellow fever research among those connected to the school.
For example, Dr. John B. Davidge, founder of UMSOM in 1807, published “A Treatise on Yellow Fever” after an epidemic in 1797. This paper became heavily cited on yellow fever and concluded that it was “indigenous, propagated by the atmosphere and non-contagious, merely a variety or aggravated form of ‘bilious remittent.’ ” In other words, yellow fever was caused by bad air. This theory of medicine was known as the miasma theory; it began in the fourth century with Hippocrates and prevailed into the 1880s when it was replaced by germ theory.
Contrarily, Baltimore doctor and UMSOM faculty member Dr. John Crawford theorized in 1790 that small particles or “animalcula” entered the human body and caused disease — an early form of germ theory. Because the miasma theory was well established, most doctors were highly critical of Crawford’s beliefs; he was forced to publish in non-medical periodicals. However, in 1848, Dr. Josiah C. Nott, a surgeon in Mobile, Ala., used Crawford’s theory and speculated that insects spread yellow fever in the article “On the Cause of Yellow Fever.” In 1881, Dr. Carlos Finlay of Cuba built on this work and discovered that a specific species of female mosquito spread the disease.
In 1898, Dr. Henry Rose Carter, an 1879 UMSOM graduate, working with the U.S. Public Health Service at a quarantine station at Ship Island, Miss., established the “intrinsic incubation theory” of yellow fever, positing that it took two weeks for the disease to incubate in the mosquito. In 1899, Carter, then assigned to Cuba, met Dr. Jesse Lazear, who began studying yellow fever while working at Johns Hopkins Hospital in 1895. Carter shared his research results with Lazear.
That same year, the U.S. Army, having lost hundreds to yellow fever in the Spanish-American War, established the Yellow Fever Commission, led by Dr. Walter Reed in Cuba. The commission included Lazear; Dr. Aristides Agramonte, acting assistant U.S. Army surgeon; and Dr. James Carroll, an 1891 UMSOM graduate who served as second in command.
The commission visited Finlay to learn about his theories and studies and was gifted mosquito larvae from him. Lazear hatched the larvae at the camp, had the mosquitoes feed on infected yellow fever patients, and then the team of doctors (minus Reed, who had returned to the United States) allowed the infected mosquitoes to bite human subjects including themselves.
Carroll was the first infected through a mosquito bite on Aug. 27, 1900. On Sept. 1, Carroll was transferred to the yellow fever ward with severe symptoms. Lazear and Agramonte sought additional verification that the mosquito caused the disease, so they subjected a private to a bite from the same mosquito. He became ill three days later. Through this, Lazear was able to confirm the incubation period that Carter theorized. Lazear, still feeling the need for additional data, infected himself with yellow fever on Sept. 13; within five days he became ill, and by Sept. 25, Lazear had died.
Read more about UMSOM's role in yellow fever research in the latest issue of CATALYST magazine.
You can read the Spring 2024 issue of CATALYST magazine, which highlights UMB's new “Climate Change, Health, and Society” elective; innovations such as the School of Dentistry's Division of Artificial Intelligence Research; Carin Cardella, public information officer for UMB Police and Public Safety who has answered the call during state emergencies; the Francis King Carey School of Law celebrating 200 years; new Health Sciences and Human Services Library Dean Emily Hurst and Chief Philanthropy Officer Greg Bowden; Fahren Nipple, autopsy assistant for the Office of the Chief Medical Examiner and assistant program director for the Master of Science in Forensic Medicine at the Graduate School; and much, much more!