Raise Your Voice: Nurses Take Patient-First Approaches to Politics and Policy
June 25, 2020 Meredith Lidard Kleeman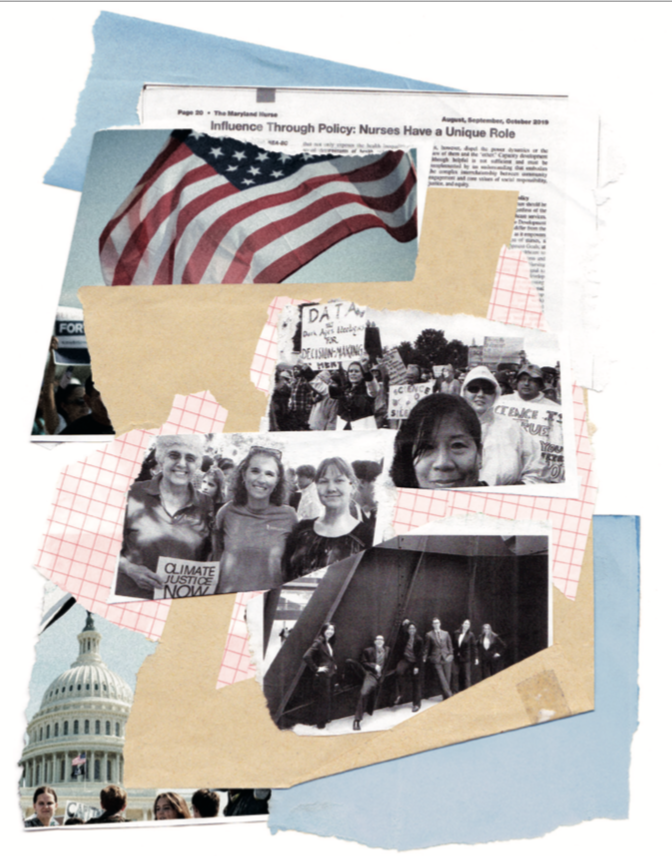
The adage “there's power in numbers” takes on new meaning when you consider nurses make up the largest group of health care providers in the United States, not to mention globally.
University of Maryland School of Nursing (UMSON) faculty, alumni, and students wield their power through political pursuits that seek to improve our nation’s health care system and patient outcomes.
No health care provider is better positioned to advocate for patients and shape the future of health care than nurses, explains Shannon Idzik, DNP ’10, MS ’03, CRNP, FAANP, FAAN, associate professor and associate dean for the Doctor of Nursing Practice (DNP) program. “Nurses tend to have the broadest understanding of all the issues,” she says. “Physicians may spend a few minutes with a patient, nurses spend several hours. Their understanding of the health care system is unparalleled.” Nurses also interact regularly with other health care professionals and understand the challenges that their colleagues face.
In an age when American politics have become increasingly partisan, nurses are finding middle ground and successes on both sides of the aisle by focusing on patient issues. Darlene Curley, MS ’82, BSN ’80, RN, FAAN, a UMSON Visionary Pioneer, is a professional policy advisor, adjunct faculty at the Columbia University School of Nursing in New York City, and former chief executive officer of Jonas Philanthropies, and she served as a representative in the Maine State Legislature from 2002-07. During her political career, Curley sought always to keep her focus on the patients. “If you put the patient first, good policy — and hopefully good politics — will ensue,” she says.
Curley notes that one of her greatest professional achievements is sponsoring and enacting a piece of legislation that penalizes habitual traffic offenders. That legislation, known as Tina’s Law, was named for a local woman who was killed by a trucker with more than 20 license suspensions, and it made Maine one of the first states in the nation to address the issue of habitual traffic offenders.
The deadly collision occurred during Curley’s morning commute to the Maine State House. After traffic came to a halt, “I hopped out of my car and could see the mangled car and truck in the median. My professional instincts kicked in, and I ran to the accident site,” she recalls, explaining that the accident’s severity shook her. “I felt inadequate because I wasn’t able to provide assistance. I learned that the victim was a neighbor and constituent. This was not acceptable, and I had a personal, professional, and legislative responsibility to advocate for change.”
Curley was also integral in passing legislation that expanded the scope of practice for nurse practitioners in Maine, and she continues to advocate for granting advanced practice registered nurses (APRNs) full practice authority in every state. To date, 22 states, including Maryland, Washington, D.C., and two U.S. territories, have granted full practice authority to nurse practitioners, permitting them to provide much-needed primary and preventive care, especially critical for patients in rural and underserved areas.
Removing barriers to nursing practice is “one of the largest achievements that we’ve made as nurses throughout the past decade,” Idzik says. In its 2010 Future of Nursing report, the Institute of Medicine (IOM) called for the removal of practice barriers preventing APRNs from providing the full scope of health care services they are educated and certified to provide. At the time, then-Dean Janet Allan, PhD, RN, FAAN, now dean emerita, reiterated the importance of this effort by saying, “We must put aside protectionist rhetoric in the interest of public welfare and give nurses the authority to do what they do best. Taking the IOM recommendations to heart means lifting practice barriers that make it difficult for nurses to get patients the care they need, such as putting nurses on provider panels and giving nurses authority to admit patients to hospitals and hospices.”
UMSON faculty have continued to advocate for implementation of full practice authority nationwide through their leadership of and involvement in organizations such as the American Association of Nurse Practitioners, the Nurse Practitioner Association of Maryland (NPAM), and the National Organization of Nurse Practitioner Faculty. Integral to this effort is ensuring that the nursing workforce is represented and that nurses’ voices are heard.
Claire Bode, DNP ’15, MS ’10, CRNP, assistant professor, serves as chair of the NPAM legislative committee and helped develop a bill introduced during this spring’s Maryland legislative session. This bill aims to increase practice authority for psychiatric mental health APRNs in emergency departments, allowing them to conduct the initial evaluation for involuntarily admitted patients.
Margaret Hammersla, PhD ’17, MS ’05, BSN ’95, CRNP-A, assistant professor and senior director of the DNP program, serves on the Maryland Health Care Commission and has proposed that nurses and APRNs be part of the commission’s panels and workgroups. “I identified that there was a lack of nurse practitioners on the advisory panel for the Maryland Primary Care Program, but there was more than sufficient physician representation,” she explains. Hammersla successfully advocated for a nurse practitioner to fill an additional seat; Cathy S. Chapman, MS ’95, CRNP, was selected.
Idzik, who served as president of NPAM from 2012-13, recalls needing to educate governmental affairs leaders for insurance companies on the importance of provider-neutral language. “They hadn’t even thought how their website, which said ‘Find a Physician,’ might create a value statement that discouraged patients from selecting a nurse practitioner,” she says.
Nurses have a professional and ethical duty to increase the access, quality, and affordability of health care, Curley explains, and nurse practitioners can address the nation’s primary care gap, but only in states that have reformed their scope of practice laws. “It’s really important for nurses to be advocates in their states to support and advance an expanded scope of practice for nurse practitioners,” she says.
Advocating for better policies is just one benefit of political engagement. As individuals, nurses are directly affected by health policies. “It affects our families, our careers, and our patients,” says Leeza Constantoulakis, PhD, MS ’14, RN, a senior associate at a leading national professional services firm. “To be stewards of our profession, we have to be paving the path to make sure tomorrow’s policies are ones that are helping us as career professionals, but also ultimately serving our patients and our patients’ needs.”
Constantoulakis felt called to pursue policy and advocacy work after attending the American Association of Colleges of Nursing’s Student Policy Summit as a student in UMSON’s Clinical Nurse Leader master’s option. “Everything came together there. I always knew I was going to have a career in health and health care, but I wouldn’t have seen how to marry it with this policy, politics, and advocacy world that I didn’t know existed, if it weren’t for the opportunities presented to me at UMSON,” she explains.
A new generation of nursing students shares Constantoulakis’ passion. Lucie Roach, a Bachelor of Science in Nursing student, serves as president of UMSON’s Students United for Policy, Education, and Research (SUPER), a chapter of AcademyHealth. She takes the long view when it comes to how nurses can improve health care. “Our health care system is for profit — that can be pretty problematic,” Roach says. “We need to work more toward universal health care, and we need to work on making health care more user-friendly.”
She knows that a nurse’s voice is powerful and integral to enacting change. “Those people making decisions need to hear from nurses,” Roach says. “If nurses don’t stand up for health care, it’s unlikely that patients are going to stand up for it.”
HOW TO GET INVOLVED
- Wade in at work. The workplace can be a great introduction to participating in policymaking. “There are many policies that take place inside of a hospital system that nurses can influence,” Constantoulakis explains. “Get on those boards within your hospital system and have a discussion.”
- We need you. Nurses should remember that when they see a call for health care commission or board members, “We mean you, we don’t mean somebody else,” Idzik says. “We want to hear your story, we want you to be on the board. If you’re reading it, you’re the people who we want to be representing nursing.”
- Volunteer. Nurses can be proactive in supporting political candidates they believe in and who support their values and priorities. “An election year is when there are the most opportunities to volunteer,” Curley says.
- Start local. It may seem overwhelming to reach out to federal legislators, but local representatives want to talk to you, Idzik explains. “They’re very easy to get ahold of,” she says. “They’re really there to represent you. The local folks are everyday citizens — they work part of the year in politics, but most of their life is being an average citizen.”
- It’s never too late. Find an organization or cause to get involved with — fresh voices and opinions are always appreciated. “Just get in touch, reach out — nobody’s going to bite, everybody’s really friendly,” Roach adds.
A Legacy of Legislation
Shirley Nathan-Pulliam, MAS, BSN ’80, RN, a UMSON Visionary Pioneer, retired from her position as a Maryland state senator in December, but her legacy
as a tireless health advocate lives on. Nathan-Pulliam dedicated her 25-year legislative career to reducing health disparities and improving health care access for all Marylanders, regardless of demographics.
She served five terms in the Maryland House of Delegates before her election in 2014 to the Maryland State Senate for the 44th District, which encompasses areas in both Baltimore City and Baltimore County.
Nathan-Pulliam advanced many policies designed to support community-based interventions. One of her key achievements during her tenure in the General Assembly was sponsoring legislation that established the state’s Office of Minority Health and Health Care Disparities in 2004. Many of Nathan-Pulliam’s legislative initiatives focused on health care, including funding for breast cancer diagnosis and treatment programs and expanding Medicaid coverage for patients with hepatitis C.
Nathan-Pulliam cites her nursing experience as integral to advancing health legislation. “Those bills I put forward probably would never have gotten passed if I wasn’t a nurse,” she says. “Nurses learn how to assess and identify a problem — I used some of those same principles in fighting for patients in the House and Senate.”
Sometimes, nurses are the only people willing to fight for patients, especially those in underserved communities. “A large number of nurses need to be involved. The legislators who make laws that impact nurses, other health care professionals, and the community — many don’t necessarily understand health care,” Nathan-Pulliam reflects. “There are many issues that I championed and took on that some of the doctors didn’t want, but nurses see things from a different perspective.”
She remains passionate about nurses running for political office. “I would encourage young nurses to run for office, and if you can’t run, be an advocate — educate your legislators on health care issues,” she adds.
THIS ARTICLE FIRST APPEARED IN THE SPRING 2020 ISSUE OF NURSING FOR/UM MAGAZINE.
ILLUSTRATION BY EMILY HAASCH
